What is it?
Lots of things can cause pain down the back of the leg. From a clinical point of view it is important for us to differentiate between Referred pain and Radicular pain, this article will try to explain that difference.
Nerves originate in the brain and track down the spinal column. Nerves that supply the lower body will have roots that branch out from the Lumbar spine (lower back). Pain travelling from the Lumbar can be Radicular (from nerves) or Referred (from somatic tissue e.g. muscles and joints).
It’s important for clinicians to identify what type of travelling pain is present to ensure the most appropriate and effective treatment. It is important to consider that these two types of pain can occur simultaneously. Sciatica is a common type of Radicular pain, outlined below is the signs and symptoms to look out for, some self-management tips and advice on when to seek treatment.
Tell-Tale signs of Sciatica
These following signs and symptoms are not diagnostic criteria, just a few things to help you understand your pain.
- Buttock Pain – The Piriformis is a deep buttock muscle that sits directly over the sciatic nerve. This muscle can spasm putting pressure on the nerve inhibiting its flow. Follow this link to our blog about why Muscles spasm.
- Sciatica is often worse below the knee – A predictor of ‘true’ sciatica (radicular pain) is leg pain worse than back pain. It is possible for some people suffering from sciatica to have no back pain, they could just have buttock or calf or toe pain. Alternatively Referred pain is worse closest to the area it’s referred from (Lower back) and gets milder the further away it gets.
- Radicular (nerve pain) – is really, really painful! But this is not necessarily a sign that there’s a more serious underlying problem or any structural damage. Referred pain isn’t pleasant either, but it tends to be duller and aching.
- There are also non painful symptoms of sciatica – buzzing, tingling, running water sensation, insects crawling, itchiness, hot or cold legs.
- Reduced but not loss – the leg may present with reduced strength, reduced sensation or dulled reflex, not complete loss. This indicates there is poor conduction higher up along the nerve. In contrast, Peripheral neuropathies (structural nerve damage) often have total paralysis of muscles, for example drop foot or total numbness in the skin. Peripheral neuropathy can result from traumatic injuries, infections or after surgery. Radicular pain is often milder than this, therefore not total loss just reduced.
- Neural sensitivity – You won’t want to stretch your nerve. Just like stretching muscles we can stretch or floss nerves, to test how supple/ flexible they are. If there is neural mechanosensitivity (Sensitivity to movement) present, a simple leg lift will be uncomfortable as this will put that nerve on stretch.
Radicular Pain
- Leg worse than back
- Neurological symptoms
- Below the knee pain
- Reduced function
- Positive nerve stretch tests
Referred Pain
- Back worse than Leg
- Poorly localised
- Dull ache
- Negative nerve stretch tests
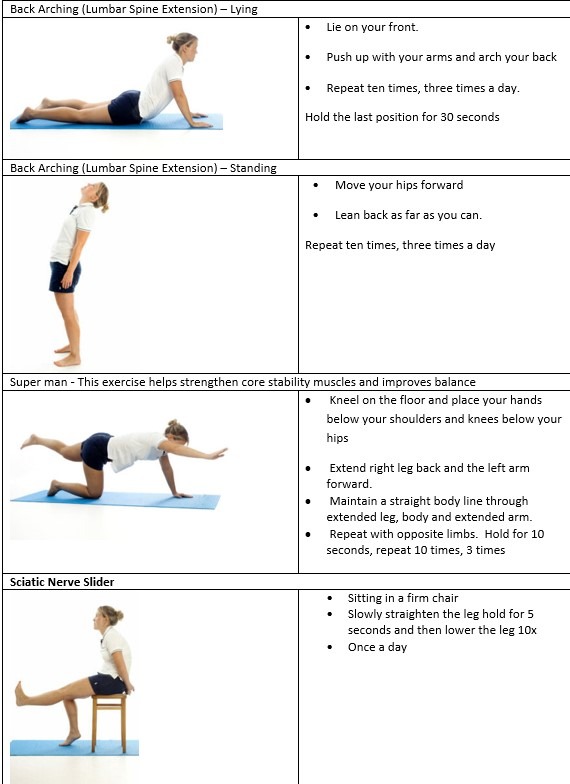
Self-management tips
These are very general home exercises; a therapist will be able to tailor these to your specific needs after an initial assessment. Please avoid any exercise or activity that makes symptoms worse and seek advice.
Please be aware of your body and take advice from your GP before exercising or send an email to enquiries@physio-logical.net for advice and guidance.
When to seek Treatment
If you are experiencing anything mentioned above, we recommend seeking some advice and physiotherapy treatment.
Any loss of bladder or bowel control or change in sensation around your saddle region (inner thigh/buttock) seek urgent medical help.
If you would like any further advice, an assessment and physiotherapy treatment can be booked online, email us: enquiries@physio-logical.net or call us on 023 9435 0270.




